
Congratulations to CCH’s first MSc graduate!
November 5th, 2018 marked a very special day in the calendar for CCH, and the future of the UK’s healthcare workforce. This date saw the graduation of our first full MSc in Obesity Care and Management student, Divya Bassi. Divya, who works for MacMillan Cancer Support, a charity, was awarded the qualification at a degree conferring ceremony at London South Bank University, which is the institution conferring the award.

Divya is shown here after the ceremony with Nigel Hinchliffe, Deputy Director of Education, at CCH and course leader in the masters programme.
The College of Contemporary Health was established in late 2013 to provide online instruction in academic and professional development courses in obesity care and management for busy health care professionals. Since that time more than 1000 students have studied various obesity-courses at CCH. It has the most complete suite of online courses in obesity care and weight management of any institution either in the UK, or abroad.
Read More
CCH Joins National Obesity Care Week 2018: Pledge to Change the Way We Care about Obesity
Today, more than 93 million Americans currently have obesity, and in the last 20 years, obesity rates have doubled among adults. It’s time to change the way we care about obesity. With obesity on the rise, our organization, alongside other organizations, must attack this disease from multiple angles and unite to overhaul the treatment of obesity. At CCH, we recognize this challenge and the important role we can play.
The 4th Annual National Obesity Care Week (NOCW) takes place October 7th through 13th, and seeks to ignite a national movement to ensure anyone affected by obesity receives respectful and comprehensive care. CCH is proud to join the Campaign, which was founded by the Obesity Action Coalition (OAC), the American Society for Metabolic and Bariatric Surgery (ASMBS), the Obesity Medicine Association (OMA), The Obesity Society (TOS) and Strategies to Overcome and Prevent Obesity Alliance (STOP).
- All NOCW supporters strongly believe that:
- Individuals with obesity must no longer be the target of weight bias in all of life’s settings, such as healthcare, employment, entertainment, and education.
- Individuals with obesity need to understand that this disease is not solely their responsibility and work with a healthcare provider to manage their obesity long-term.
- Like individuals with other chronic diseases, individuals with obesity must have access to and coverage of science-based treatments to improve their weight and health.
- Healthcare providers need to be trained to provide effective, compassionate science-based care and use of shared decision-making.
- Providers and policy makers must recognize the need for further investment in the education, prevention and treatment of the disease of obesity.
Although it is important to educate people about these reasons to care, we must also address barriers to care such as weight bias in both society and among the medical community. We need more voices – your voice – to reach our goal of achieving better care. You can join us and pledge to take ACTION to Change the Way We Care about Obesity.
Additional information about National Obesity Care Week and ways to take ACTION, including information and resources, is available on ObesityCareWeek.org/ACTION.
Mark your calendars, and join us in recognizing National Obesity Care Week, October 7th – 13th, 2018.
Read More
5 Resources All Health Professionals Should Know About
A lot of resources that are available for healthcare professionals (HCPs) are outdated, too commercial, and lack trust from the HCP community. But there are some hidden gems however, especially concerning the fields of modern health conditions, that we believe will be beneficial for those who utilise them.
1. Professr
Have you ever wanted somewhere other than Facebook to communicate with fellow health professionals?
Professr is UK based digital startup with a dedicated platform for health professionals to communicate and network with one another.
The platform is provided as a free resource to health professionals, with the intention of encouraging multidisciplinary communication and helping health professionals to support each other in an increasingly high pressure healthcare environment. This is particularly important for those who are newer to their field of practice (i.e. junior doctors), or those who work in remote or isolated conditions (i.e. outreach workers).
Professr’s forum-like features allow members to upvote and downvote answers to questions relating to healthcare, creating a repository of community-rated information. Having an opportunity to gain insights with professionals from multiple disciplines enriches the perspective of a health professional and can aid in providing better outcomes for patients.

2. CCH Toolkits
The College of Contemporary Health (CCH) is renowned as the leading global educator for obesity. They offer a range of course types including postgraduate courses and modules, short courses and on-demand courses. The short courses and on-demand courses both offer continuing professional development (CPD) credits which can be used to build professional standing, while the postgraduate options are ideal for healthcare professionals who are looking to further develop their skills and understanding in weight management and obesity care.
Besides a full range postgraduate and short courses, CCH has developed an ever growing range of toolkits. CCH toolkits are designed to be used as handouts for health professionals who can use them for themselves, or distribute to their patients.
These toolkits are easily available, open for the public, and completely free. Here you will find resources associated with health, weight management, nutrition, sleep, fatigue, mental health and many other contemporary health issues that you can refer to, and use, both personally and professionally.
The CCH Team are committed to building a comprehensive library of resources, and are constantly updating their website with new toolkits, so be sure to come back frequently or subscribe to CCH’s mailing list and have new toolkits delivered to your mailbox monthly.
You can sign up here: https://www.contemporaryhealth.co.uk/preferences

3. Conferences (Diabetes Professional Care)
Conferences are an excellent resource for health professionals that are often not utilised enough. They provide a great place to network, learn from industry leaders, and build relationships with those who share a passion for the same field of health you practise in.
Although conferences can sometimes be rather pricey to attend, some of the best ones, are in fact, free. An example of a great free-to-attend conference is Diabetes Professional Care (DPC). DPC is the is a unique, free-to-attend, CPD-accredited event for healthcare professionals (HCPs) involved in the prevention, treatment and management of diabetes, and its related conditions. Launched in 2015, DPC meets a real and increasing need for accessible education among HCPs by arming them with the skills and knowledge to provide better care for their patients.
DPC2017 attracted a record attendance of 3,235 visitors – and DPC2018 promises to be even bigger and better. So, if you’re a professional responsible for delivering diabetes care pathways at any level, it is the one event you can’t afford to miss.
This year’s DPC is on the 14th and 15th of November in London’s Kensington Olympia.
You can find more information here: https://www.diabetesprofessionalcare.com/

4. BMJ Best Practice
Healthtech is a constantly growing field and isn’t just limited to our two previously mentioned healthtech innovators such as great social platforms like Professr, and forward thinking online education institution, the College of Contemporary Health.
Instead, there has been an emergence of tools that help personal performance as a health professional and aid practice. One such tool is BMJ Best Practice.
BMJ Best Practice is ranked one of the best clinical decision support tools for health professionals worldwide. It takes you quickly and accurately to the latest evidence-based information, whenever and wherever you need it. They provide a step-by-step guidance on diagnosis, prognosis, treatment and prevention that is updated daily using robust evidence based methodology and expert opinion. Their goal is to support you in implementing good practice.
You can find more information on BMJ Best Practice here: https://bestpractice.bmj.com/info/

5. Podcasts. (Dr Chatterjee’s Feel Better, Live More)
In the field of health, there are always new developments and information that health professionals are constantly being bombarded with, and in many cases, just don’t have the time to read, watch, or catch up with. Podcasts are an excellent way of keeping up-to-date with the latest information without having to invest a huge amount of time or focus doing so. Podcasts can be listened to passively while you’re commuting, doing the washing up, or whatever mundane task you may be performing.
Our podcast pick is Dr Chatterjee’s Feel Better, Live More. It covers a range of topical issues in health, usually with highly influential guests who are experts in the area being covered. Topics have ranged from childhood obesity with Jamie Oliver, to brain nourishing foods with neuroscientist, Dr Lisa Mosconi.
The podcast is usually released on a weekly basis so it can fit into your busy schedule, perhaps your Monday morning commute.
For more information please click here: drchatterjee.com/blog/category/podcast/


Type 2 Diabetes Prevention: 10 tips for empathic communication about excess weight
Overweight and obesity have increased significantly in the UK over recent decades, with more than half of all adults and a third of children now affected. The reason this is of such concern and one of the biggest public health issues of modern times, is that excess weight, particularly in the form of fat carried around the middle (abdominal fat), greatly increases the risk of a number of non-communicable diseases, most notably Type 2 diabetes mellitus (T2DM) and cardiovascular disease (CVD).
It is therefore important that weight management is promoted in all areas of healthcare, particularly for people who have, or are at risk of, T2DM or CVD. The cornerstone of any diabetes prevention programme is weight management through promotion of healthy eating and physical activity.
The first step to helping people with weight concerns is to initiate a conversation about their weight. This is not as simple as you might think, from the perspective of the practitioner. Healthcare professionals can find it uncomfortable to raise the issue of weight, and sometimes feel they lack the skills to do so.
On the other hand, patients can also be reluctant to talk about their weight. While recent evidence suggests that most patients with excess weight are happy to discuss their weight and opportunities for weight loss (Aveyard et al. 2016), this is not true for everyone. Some people can feel embarrassed, guilty or ashamed of their weight.
So what can we do to overcome this problem? How can we raise the issue of weight in a way that facilitates patient-practitioner interactions that are both productive and positive experiences?
The most important thing is to always communicate sensitively, using appropriate language, terminology and attitudes, to make the patient feel comfortable and positive about the conversation. In fact, skilled communication by the clinician can not only enhance patient understanding and trust, but also lead to increased adherence to programmes and ultimately improved health and well-being (Street et al. 2009).

Healthcare professionals can find it uncomfortable to raise the issue of weight, and sometimes feel they lack the skills to do so.
Here are some tips to communicating sensitively and empathically about weight:
1. Ask permission to talk about weight, for example; “Would you mind if I spoke to you briefly about weight management?” This immediately gives control to the patient – they decide if they want to discuss their weight or not.
2. Be aware of the language you use and try to avoid language which may be perceived as negative eg fat, obese. Terms such as excess weight and BMI are generally better received.
3. Be prepared for a wide range of responses. The subject of weight can be a highly sensitive one and produce a variety of emotions and reactions including denial, disinterest, shame and relief.
4. Work on responding constructively to all types of responses. Keep body language and facial expressions, as well as verbal language, positive and constructive.
5. Listen attentively to the patient’s story. General tips for listening include: Ask open ended questions; Do not interrupt the patient; Maintain eye contact; Do not take notes or look at your computer.
6. Communicate empathy, compassion and support. Try to see the world through the patient’s eyes, which is very different from a clinical diagnosis of illness. It can provide a framework for approaching their problems holistically, and uncover diagnostic and therapeutic options.
7. Discourage patients from feeling a sense of guilt. Acknowledge the societal nature of the problem and the influence of the obesogenic environment, which promotes overeating and physical inactivity.
8. Avoid telling the patient what they have to do. As health professions we often have a strong drive to set things right when we see an individual may be doing something that is detrimental to their health. This typically manifests as advice based on how we see the situation, and the more we try to advise or guide an individual the more we can polarise our relationship with them and fail in our attempts to help.
9. Empower your patient. Explore how your patient can make a difference to their weight themselves. Their own ideas about how they can implement changes into their own life are critical. Emphasize their strengths and opportunities for change.
10. Provide clear and accurate information – verbally, visually and/ or in writing. It is vital the patient goes away with a clear understanding of the issues relating to their weight and health.
References
Aveyard P et al. (2016) Screening and brief intervention for obesity in primary care: a parallel, two-arm, randomised trial. The Lancet. 388: 2492-2500.
Street RL Jr, Makoul G, Arora NK, Epstein RM (2009) How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 74: 295-301.

What is the Solution to the Diabetes Crisis?
What is the solution to our diabetes crisis? Just how do we prevent diabetes?
Last week in the UK, from the 16th to the 22nd of April, was Diabetes Prevention Week. The NHS, as part of their very own Diabetes Prevention Programme, set up the event in the hopes of raising awareness of the disease and their Healthier You programme. Diabetes Prevention Week provided an excellent chance to spread awareness of a disease that most people don’t really know anything about. The word diabetes for some brings up images of sugar-free diets, insulin injections, and in some cases, the possibility of losing limbs, but that’s about it. Unfortunately, most of the public are unaware of many of the details of the disease, from the 2 different types, to the causes of each type, or the impact it can have on the lives of those it affects, and that should certainly change. But besides campaigns such as this one by the NHS, what has actually been done, or even proposed, as a measure to help prevent diabetes? And, how do we prevent diabetes? Is it even possible?
To fully appreciate Diabetes Prevention Week you have to first understand the disease of diabetes. Not everyone knows, but there are two very different types of diabetes, type 1 and type 2. Type 1 is an autoimmune disease, which means that the immune system mistakenly attacks parts of the body rather than protecting them, and in the case of type 1 diabetes, the immune system attacks insulin producing beta-cells in the pancreas. This means that those with type 1 diabetes are incapable of producing insulin, making them insulin dependent, requiring them to inject themselves with insulin to compensate. It is not fully understood what the cause of type 1 diabetes is, however it is believed that both genetic and environmental factors are involved.
Type 2 diabetes is entirely different to type 1. The autoimmune system of those with type 2 diabetes functions properly, and instead of being insulin dependent like type 1 sufferers, type 2 sufferers are insulin resistant. Their bodies lose the ability to respond to insulin. The body compensates for the ineffectiveness of its insulin by producing more, but it can’t always produce enough. Over time, the strain placed on the beta cells by this level of insulin production can destroy them, diminishing insulin production. Around 90% of all diabetes cases are type 2, and the vast majority of them are caused by overweight or obesity. Although, it is believed that in some of these cases genetic factors are also involved.
Download our toolkit for reducing your risk of type 2 diabetes here: https://www.contemporaryhealth.co.uk/portfolio/reduce-the-risk-of-developing-diabetes/
Public awareness of the disease is a great tool in its prevention, however, governments across the globe are taking it upon themselves to develop and implement policies that will help reduce the numbers of those developing it even further. In Singapore for example, the Ministry of Health has outlined plans that they say will directly combat diabetes. Included in this plan is the installation of more water fountains in public places to wean people off sweet drinks, competitions to promote cooking healthy food, engaging with celebrities to promote healthier eating, restrictions on fast-food and snack advertisements, and giving out health points and travel rebates to encourage physical activity. It will certainly be exciting to see the results of this extensive plan, and just how preventative the proposed strategies prove to be.

The Singapore government will be implementing a new strategy to prevent diabetes.
In the UK, the National Health Service spends £12 Million a year treating those with the disease. This figure has united members of parliament and health professionals alike, to act immediately on the crisis. Tahseen Chowdhury, a specialist in diabetes and metabolism at Barts Health NHS Trust in London, suggested that “the NHS should put people with type 2 diabetes on drastic diets to reverse the condition, instead of spending billions of pounds trying to treat it.” Members of parliament have suggested recently that good preventative measure would be to restrict the advertising of junk food even further than it already is, and outlaw offers and deals on junk food that seem to be prolific in every major supermarket.
All aforementioned preventive measures by governments, MPs and members of the public, focus on diet and weight management, so why do we focus so much on diabetes prevention and not obesity and overweight prevention? Type 2 diabetes can be prevented and in some cases reversed, while type 1 can’t, so it’s misleading and confusing to have a Diabetes Prevention Week, when only one form of the disease can actually be prevented.
We should instead have an Obesity Prevention Week, as it’s impossible to prevent type 1 diabetes, but type 2 diabetes, which makes up 90% of all diabetes sufferers, can be prevented through effective weight management and lifestyle intervention. Not only will raising awareness for preventing overweight and obesity help prevent the majority of type 2 diabetes cases, but the whole range of comorbidities that come with overweight and obesity such as: heart disease, non-alcoholic fatty liver disease, metabolic syndrome, gout, sleep apnea, cardiovascular disease, hypertension, and many different types of cancer.
We will only ever have a solution to the diabetes crisis when we have a solution to the obesity crisis.
Read More
Junk Food Advertising: How Much is Too Much?
Last week saw the implementation of the “sugar tax.” It is one of the first big government initiatives here in the UK aimed specifically at dealing with the obesity epidemic with the hope of improving public health. Despite this initial effort from the government, many are calling for even more action to be taken with some pointing their fingers squarely at the advertising industry. It’s believed that the sheer amount of advertising for sugary, salty, and high fat junk food is excessive, targets children unfairly, and promotes poor diets and ill-health. With obesity and childhood obesity numbers continuing to soar, do those who wish to see a limit on junk food advertising have a point?
Although a declining medium of entertainment, especially among youths, television is still the biggest forum for advertisers to get their message to as much of the public as possible. Prime time television in the UK can still draw huge numbers of viewers with programmes like The Voice attracting 5.6 million viewers for its 2017 season premiere. Out of that 5.6 million people, roughly 710,000 children were viewers, with Liverpool University appetite and obesity researchers finding that those children faced no fewer than 12 junk food ads during the hour, with ads for Domino’s pizzas, McVitie’s chocolate digestive nibbles, and Anchor spreadable butter making up just a few. Experts who looked at the data collated by the Liverpool University researchers claimed that children were being “bombarded” with junk food ads and that a minimum of a 9pm watershed on these adverts was necessary, saying current guidelines were “failing children”.

Technology and the internet will continue to have an ever-growing influence on children.
As more and more children begin to abandon television for more portable forms of entertainment like mobile phones and tablets, it is only necessary that we should turn our attention to the presence of junk food advertisements on those devices. Social media, media platforms like Youtube, and many other popular websites frequented by the public and children are often strewn with junk food ads. Research in Canada discovered that over 90% of food and beverage product ads viewed by children and youth online were for unhealthy food products. Although those figures were for Canada, it is hard to imagine that it’s much different in the UK where the culture and obesity figures are similar.
Junk food advertising doesn’t just stop once the screens are off. Anyone who has been to a supermarket recently will know that the offers for junk food are ubiquitous with every aisle enticing customers to be upsold on energy dense, nutrient poor junk food. Even their placement at supermarket checkouts are strategic in their lure to get the public to act on their impulse and make a thoughtless, unnecessary purchase of something unhealthy. This however, has not gone unnoticed by members of the health conscious public as a committee of MPs, as recently as 2017, put forward a plan to restrict supermarkets from offering “deep discounts” on a variety of unhealthy foods, especially junk food. There has also been pushback on just where in the supermarkets junk food should be sold with the Department of Health putting forward a code stating “that in retail stores with more than four checkout lanes, a minimum of one should be free of junk food.” Despite these being a step in the direction towards a healthier public, they are all optional for retailers, and whether or not they participate, is up to them.
Despite the call for junk food advertising bans, there are however some junk food advertising restrictions already in place. Since July 1st 2017 advertisers were no longer allowed to show online ads for food and drinks high in fat, salt or sugar in all media where under-16s made up a quarter of the audience. Other restrictions also include the current rules, introduced in 2007, that bans the advertising of high-fat, high-sugar foods during children’s TV programmes or any programme where 75% of the audience will be children. Just yesterday, The Times reported that, “junk food advertisements would be blocked on social media under plans being drawn up in the fight against obesity,” and that, “curbs on advertising junk food, including a 9pm watershed, were being worked on in Downing Street after Theresa May reversed her opposition to restrictions on marketing.”

Junk food fills a shopping trolley at a supermarket.
So, some calls for junk food advertising restrictions are being heeded, and new restrictions would mark a big change for junk food advertisers, but some believe in extending those even further with prized neuroscientist, Wolfram Schultz, believing that selling junk food in plain packaging could help even further in the battle against obesity. He believes that, “the colourful wrapping and attractive advertising of calorie-rich foods encourage people to buy items that put them at risk of overeating and becoming obese in the future.” Despite this seeming like quite an extreme measure, it has been implemented for cigarettes in some countries like the UK and Australia. However, this seems unlikely to change for junk food any time soon.
Government imposed restrictions on junk food advertising are a great tool in helping the public to make healthier food choices, but if there is to be real change it also needs to come from the networks and platforms who display the advertisements. A glimmer of hope was recently seen in the United States when, in 2015, an independent initiative from Disney brought a self-imposed ban on junk food advertising on any of its TV channels, radio stations, and websites intended for children. It was the first major media company in which to do so.
The most effective change will come when both government and business act responsibly and work together to reduce the amount of unhealthy junk food advertising that the public is constantly exposed to.
Read More
The 3 Most Innovative Government Plans to Tackle Obesity
Today, here in the UK, is a monumental day for public health. April 6th marks the debut of the much deliberated, and heavily debated, implementation of what is now commonly known as the “Sugar Tax.” This means that from today, the UK’s tax on sugary drinks will see shoppers being asked to pay 18p or 24p more a litre, depending on just how much sugar has been added to their drinks. The hope is that either the consumer will be put off by the higher price of the product, or the manufacturers will have more incentive to reduce the sugar content of their goods. Both outcomes are a big win for public health. Despite this being a big day for public health in the UK, taxing unhealthy products, like cigarettes, making them more expensive and off-putting for consumers is a strategy that has been around for years and hardly innovative. If the UK’s government is to make any serious impact on the obesity epidemic it should take a look across the globe to see how other governments are implementing new and innovative strategies to tackle the same epidemic it faces. Here are 3 of the most innovative government plans developed in order to tackle obesity.

Albert Cuyp Street Market, Amsterdam.
Amsterdam: Amsterdam is a city filled with limber cyclists and walkable streets next to beautiful canals, so it comes as a big surprise to learn that it has the highest rate of childhood obesity in the Netherlands. In 2014, the proportion of 5-year-olds in Amsterdam who were overweight or obese stood at 13.9%. Politician Eric van der Burg took it upon himself to help Amsterdam achieve the lofty goal of not a single child in Amsterdam with obesity by 2033 with a city-wide anti-obesity campaign. The campaign mandates that children are now weighed and measured at school every year, despite parents’ initial objections. Children in certain schools are banned from bringing sugary drinks like squashes and juices to campus, and instead may only bring water and milk. Students are also presented with vegetables like carrots and radishes, and instructed that they must at least try them. Amsterdam now also refuses funding for events that are sponsored by McDonalds or Coca-Cola, whose junk food message doesn’t comply with the anti-obesity campaign.

Downtown Doha, Qatar.
Qatar: Qatar is a tiny Gulf state known for its rich natural resources and as the future hosts of the 2022 FIFA World Cup. Despite its great wealth, Qatar is battling a serious public health crisis with obesity and its comorbidities with 7 out of 10 Qataris either overweight or obese, and almost 1 in 5 with diabetes. Later this year, Qatar is set to become the first country in the world to start screening its entire adult population for diabetes, one of the most deadly comorbidities of obesity. On top of this screening initiative, the National Diabetes Committee has started to use other less conventional channels to help get their healthy message to more of the public. They are helping to educate Imams on how their weekly sermon can help improve the lifestyle of those in attendance by using examples from religion.

Boats on the shores of Vanuatu.
Vanuatu: Vanuatu is a small archipelago nation in the South Pacific off the east coast of Australia. It is mostly known for its coral reefs, great scuba diving, and white sandy beaches. However, it is beginning to gain a reputation as one of the most obese nations in the world with 28% of the country’s residents suffering from obesity according to the World Health Organisation. The Vanuatu government has decided to pinpoint what it believes is the cause of the problem and take direct action. Western junk food is believed to be the prime culprit in the explosion of obesity on the island and the plan is to ban it at government events and tourist spots in one of its provinces, Torba, to help curb rising obesity. In place of the junk food in Torba it aims to be the first organic province by the year 2020 with residents utilising locally grown or sourced food exclusively to sustain its population including fish, crabs, shellfish, taro, yams, paw paw and pineapple.
To learn more about obesity, its prevention, and its treatment please look at CCH’s Postgraduate Academic Courses in Lifestyle Medicine (Obesity Care), and CPD Short Courses in topics such as childhood obesity and behaviour change, designed to up-skill health professionals in this vitally important, and often overlooked, area of care.
Read More
Cooking Up a Solution to the Obesity Crisis?
As the global obesity epidemic continues to escalate, different solutions are put forward every day by governments, private organisations, charities, and members of the public. Of the many varying solutions that are suggested, one, in particular, seems to have gained a lot of traction in the last couple of years; cooking classes. It is said that due to the obesogenic environment we live in, and both the stresses and conveniences of modern life, that the art of cooking, is a dying one. Time constraints and modern conveniences have seen a surge in the consumption of highly processed, high calorie, energy-dense food, and a plummet in people taking the time to cook, exercise and take part in other physical activity.
The argument for cooking classes is the idea that it will bring the public back into the kitchen where they will rekindle their love for fresh, healthy ingredients and homemade taste, whilst also getting more physical activity in the process. Cooking classes as a treatment for individuals with overweight and obesity is not a new idea, and has actually been in existence since early 2017 when the National Institute for Health and Care Excellence (NICE), and the NHS Diabetes Prevention Programme: Healthier You, both published guidelines suggesting, amongst other things, that cooking classes should be an option for those who are seeking to make drastic lifestyle changes in order to help treat, and even reverse, their obesity.
Adult cooking classes for individuals with overweight and obesity seem like a good idea, but that doesn’t mean it wasn’t greeted with its fair share of scepticism with Guardian columnist, Hugh Muir, stating “Cookery courses for obese people are pointless, and ministers know it.” Mr. Muir believes that cooking is no solution to the obesity crisis and that instead, it is government intervention and policy that should be the solution. What he fails to realise is that there is no single solution to such a complex problem and that government intervention, cooking classes, and a host of other obesity prevention initiatives are the answer.
Cooking classes have not just been recommended as a treatment strategy for adults with overweight or obesity, but also as a part of the preventative strategy for children as well. Many children growing up in the 21st Century have been surrounded by cheap takeaways and ready-made, or frozen, meals which have contributed to the rise of childhood obesity levels to unprecedented highs, and has left some children incapable of preparing any type of fresh meal. This includes every step of the process, from buying the raw ingredients at the supermarket, to preparation, and to finally cooking it. The idea was first proposed in the UK in 2008 by then Schools and Children Secretary, Ed Balls. He said, “Teaching kids to cook healthy meals is an important way schools can help produce healthy adults.” Eating habits, and education on nutrition, are certainly vital and necessary skills that our young people should be equipped with if they are ever to have a chance of remaining a healthy weight in our present environment.
Both Muir and Balls had very strong opinions on the helpfulness of cooking classes in the face of the obesity epidemic, but, neither had any evidence to help strengthen their positions at the time. Despite the scepticism, cooking classes have provided promising results as released for the first time this week by the NHS. Their diabetes prevention programme, Healthier You, introduced cooking to adults with obesity as part of a treatment plan and it was found that, “overweight people who attended NHS exercise and cookery classes lose an average of half a stone” Despite these results only being preliminary, it is certainly promising news for the fight in the obesity epidemic, and a great tool for helping us to reshape the way in which we can think about tackling it.
What’s important to remember, however, is that cooking classes will only truly be useful to the public if they have a professional help them understand the nutrition behind the meal they are preparing. However, given the level of nutritional education in current medical training, that will be a tall order. According to recent research, there is a “severe deficiency in nutrition education at all levels of medical training.” The foundational links between nutrition and weight management need to be understood by health professionals if we are to be serious about reversing the current worrying trends of overweight and obesity with the public. The College of Contemporary Health’s Nutrition and Weight Management short course was designed specifically to help rectify the lack of nutritional education that our healthcare professionals need. Cooking classes and health professionals with more robust and up-to-date nutritional education, together can take the public fight against the obesity epidemic a step in the right direction.
Read More
Cancer Research UK’s Obesity Campaign Causes Online Backlash
Smoking. Everyone knows the risks involved and the impacts it can have on your overall health. The links between smoking and emphysema, coronary heart disease, and in particular, cancer, have been long established and well publicised for decades. It is the biggest cause of preventable cancer cases in the UK, but perhaps what isn’t as widely known, and in this case, accepted, is what comes as a close second to smoking, and that is obesity. According to Cancer Research UK, “it’s thought that more than 1 in 20 cancers in the UK are linked to being overweight or obese,” and what is even more alarming is how little the public is aware of this fact with the same charity also stating that “being obese or overweight is linked to 13 different types of cancer, but only 15% of people in the UK are aware of the connection.”
Cancer Research UK took it upon themselves last week to inform the public of this health epidemic with a hard-hitting campaign that has been published on billboards and advertising space all over London and the rest of the UK. The campaign, designed in a “hangman game” style format, had the word obesity written in large font with letters missing from the word in order to make the public think, and guess, for themselves as to what the full word might be. What made the campaign especially hard-hitting is that it was designed in the exact same format found on cigarette packets which plainly details the, often gruesome, health risks involved with smoking. Using this format was an excellent way to effectively demonstrate that smoking and obesity can be as potentially dangerous as each other in causing cancer, and in both cases, lifestyle changes can be an effective preventative measure for developing the disease.

Cancer Research UK campaign advertisement seen in Peckham, London.
As the campaign made its physical presence felt, filling bus stops, tube stations, and various other advertising spaces around the UK, a quite unexpected backlash took hold on social media and discontent was soon voiced, and in many cases, sheer outrage emerged. Perhaps the loudest voice among the discontented was Danish comedian, Sofie Hagen, who, amongst other things, deemed this campaign as “hate.” Ms Hagen posted a series of tweets highlighting her outrage at the bold campaign from Cancer Research UK.
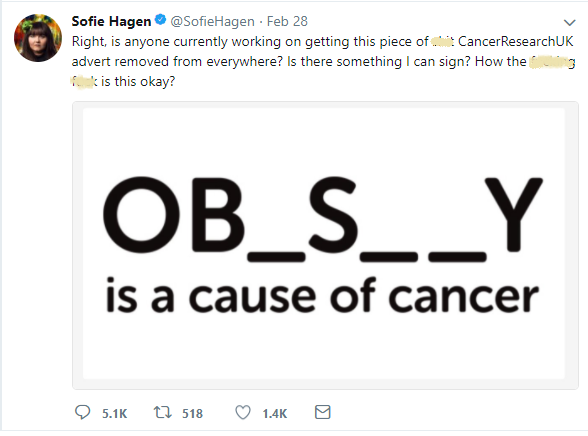
After imploring this campaign to be removed, even though it hadn’t even been present for a day, Ms. Hagen explained as to why she thought that it was so offensive and this was because, as she describes, “it uses shame, ridicule, abuse, and fear” in order to get individuals with overweight or obesity to “change their ways.” Many of Ms. Hagens followers agreed with her with one adding that “There is a difference between informing and shaming and THIS campaign shames.” Some were so enraged by Cancer Research UK’s campaign that they encouraged the public to never donate to the charity ever again and to only donate to charities that don’t body shame.
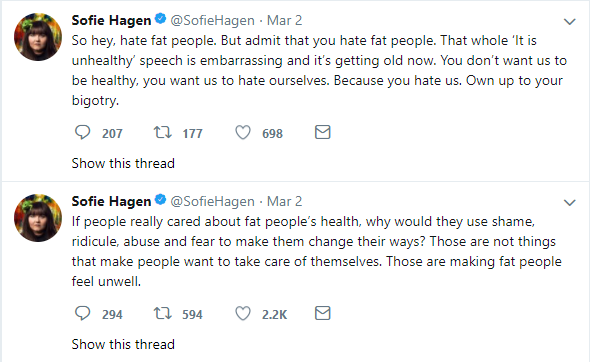
The outrage that this campaign attracted has drawn many questions, but one particularly pertinent question sticks out, and that is as to what exactly constitutes body shaming. Cancer Research UK’s campaign featured no people of any description in any of the variations of the advertisements. It only promoted the fact that after smoking, obesity is the biggest preventable cause of cancer, and was trying to make the public aware of this. So why was there such outrage? The outrage was probably due to the fact that obesity is an extremely sensitive topic and often the language used surrounding people with overweight or obesity is insensitive and counterproductive. There is no doubt that the way we talk about obesity needs improvement and should change, however attacking what is supposed to be an informing, and moving, campaign by a reputable national charity is not the way to do it.
The way to achieve a real change in the way we talk about obesity is to start using tools like People First language that the College of Contemporary Health was recently recognised for. People-First language is not something new; however, it is new to the obesity community. It separates the individual from their disease rather than labelling someone as their disease. For example, instead of using “the obese man was elderly” use, “the man with obesity was elderly.” People-First language, healthcare professionals trained in obesity care, and an awareness of obesity brought to the public by campaigns like this one by Cancer Research UK, is what will prompt real change in the way we perceive obesity in society and treat individuals with the disease.
To learn more about obesity, its prevention, and its treatment please look at CCH’s Postgraduate Academic Courses in Lifestyle Medicine (Obesity Care), and CPD Short Courses in topics such as childhood obesity and behaviour change, designed to up-skill health professionals in this vitally important, and often overlooked, area of care.

CCH win Southwark Healthy Weight Training Contract
Innovative online education company to support London Borough attain a healthy weight
London, UK: The College of Contemporary Health, an online college specialising in innovative e-Learning for health professionals in weight management and obesity care, are excited to announce that we have secured the opportunity to partner with the London Borough of Southwark and develop online courses for health professionals and community members in the Borough.
Southwark has some of the highest rates of obesity in the country with 47% of all adults and 43% of children in year 6 classified as overweight and obese. Overweight and obesity not only impacts the quality of life of Southwark residents but also on their productivity and health.
Southwark Council is committed to delivering its vision to make Southwark a safer and healthier place and CCH is delighted to be collaborating with Southwark to improve the health of the local population and to help them achieve that goal. CCH will do this by providing a bespoke e-learning offering for the Borough.
CCH are experienced providers of continuing professional development (CPD) accredited e- Learning and will be developing 2 unique courses for health professionals and community members across the London Borough of Southwark.
I am delighted that CCH has secured the tender for this exciting and innovative project within the Borough of Southwark. With fewer than 0.1% of health professionals in the UK having any training in the critical public health area of obesity, it is great to be partnering with an organisation who is keen to make a difference. We are excited to be offered the opportunity to deliver courses that will better equip health and community members in Southwark.
Daniel Pothecary-Smith, Business Development Executive, CCH.
About College of Contemporary Health (CCH): College of Contemporary Health is an e-Learning college providing accessible online training for health professionals in weight management and obesity care. All CCH courses are evidence-based, use a learner centred approach and are overseen by an esteemed Academic Advisory Board. CCH have trained health professionals across the UK and globe and provide the only completely online Masters in Obesity Care and Management.
Read More
Starting an online Masters – Do you know what to expect?
What do I need to consider before starting?
Studying at master's level does require a higher level of commitment. To get the most out of your studies, it is important that you set time aside to read and study the materials. CCH's MSc in Obesity Care and Management is made up of presentations, videos, podcasts and reading materials to complement, and suit, all learning styles.

Who will I be studying with?
You will be studying with fellow health professionals from across the UK and the globe including: GPs, doctors, nurses, physicians, surgeons, physiotherapists, dieticians, nutritionists, psychologists and professionals working in weight management. Our international student base means that you have the unique opportunity to share best practice with health professionals from across the globe!
Will I get support?
CCH student support is second to none. From online tutors and module leaders, assisting you to achieve your best academic potential, to an in-house tech and admissions team to help you with any query you have – no matter how big or small! You will be completely supported throughout your time at CCH.

Will it even be worth it
Absolutely! Studying the Masters in Obesity Care and Management prepares you for the challenges that patients with obesity can present. The course gives you the tools, skills and confidence to provide your patients with the best evidence-based obesity care and weight management.
What can I do after studying?
The MSc Obesity Care and Management prepares health professionals for a leadership role within weight and obesity management. This includes: GPs, doctors, nurses, physicians, surgeons, physiotherapists, dieticians, psychologists, and counsellors running weight management clinics. On completing the MSc you will have the knowledge and skills to further improve patient care which could enhance your future career progression.
Click here to apply
for the MSc in Obesity Care and Management and take that first step to becoming an Obesity Specialist today.

MPs calling for reduction in multi-buy offers
A group of MPs have urged the government that more must be done to reduce the number of multi-buy offers on unhealthy foods to help curb childhood obesity. Further to this, they say that rules on junk food advertising must get more stringent and clear, claiming that the current obesity plan set forth by the government is too vague. The British government announced a childhood obesity plan in 2016, one of the main points was the sugar tax, however many in the wider health community have criticised this plan saying that there must be more action.
In the latest Health Select Committee report, the MPs are calling for more to be done to stop big discounts on unhealthy food and therefore halt their promotion towards children. This comes after evidence from the food industry that responsible retailers are being undercut by those who continue to offer attractive discounts. Whilst some supermarket chains have reduced the number of deals that they promote, many others are still pushing theirs forward. The British Retail Consortium has stated that there will have to be industry-wide agreement if junk food promotions were to be reduced, and this is an incredibly difficult thing to implement.
The MPs also suggested that more must be done to stop junk food advertisements to children. Currently, these types of adverts are banned during programmes that are aimed at children, the MPs suggest that they should be banned during all programmes that children might watch as well. They go on to propose that the sugar tax should extend to milk-based products that are currently excluded but still contain added sugar. Whilst they are aware that many of these plans are ambitious, they are keen to point out that more must be done to stop the development of childhood obesity, and only by implementing new plans and strategies can this be achieved.
Read More