
Nutritional studies highlight pulses as key to lowering diabetes and cholesterol risks
Research consistently highlights pulses—such as beans, peas, lentils, and chickpeas—as crucial allies in the fight against diabetes and elevated cholesterol levels. This insight comes at a critical time, as projections from a study published in The Lancet last year forecast that diabetes could affect over 1.31 billion people globally by 2050. Concurrently, elevated cholesterol levels remain a significant health issue, with nearly half of adults in the UK exceeding national guidelines.
A detailed review in the journal Nutrients has shown that regular consumption of pulses can significantly improve these concerning health trends. The review meticulously examined thirty studies that looked at various types of pulses, including lentils, chickpeas, and several common beans like pinto, black, and kidney beans. The studies covered a wide array of health outcomes, from lipid profiles and blood pressure to risks of cardiovascular diseases and diabetes management.
The findings from these studies are telling. They specifically note improvements in low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol, systolic and diastolic blood pressure, fasting blood sugar, haemoglobin A1c levels, waist circumference, and markers of inflammation and sensitivity such as C-reactive protein. These outcomes particularly underscore the potential of pulses to enhance lipid profiles and manage blood pressure.
The review emphasised that interventional studies, which typically have larger sample sizes and provide robust data, consistently confirm the health benefits of pulses. These studies often involved dietary adjustments where pulses replaced red meat or were added to diets as fixed servings. The results repeatedly demonstrated improvements in dietary quality and beneficial health outcomes.
Pulses’ potential to prevent heart disease is particularly noteworthy, largely due to their ability to lower total and LDL cholesterol levels. The authors of the review highlight that pulses are low in fat and rich in healthy mono- and polyunsaturated fats, essential micronutrients, and bioactive compounds with antioxidant properties, making them a true “nutritional powerhouse.”
Longitudinal studies also link higher pulse consumption with reduced risks of developing type 2 diabetes. This association is bolstered by interventional studies that document notable improvements in fasting glucose levels and insulin sensitivity with increased pulse intake. Consequently, pulses are not only pivotal in preventing diabetes but also in managing blood glucose levels effectively.
Tim McGreevy, CEO of USA Pulses, commented on the research, stating, “This research accentuates the fact that pulses are beneficial for health in so many ways, underscoring dietary guidelines that endorse plant-based eating patterns,” even though he was not directly involved in the study.
Additionally, awareness about type 2 diabetes is critical as many individuals may be unknowingly afflicted. Symptoms to watch for include increased urination, persistent thirst, excessive tiredness, unexplained weight loss, genital itching or recurrent thrush, delayed healing of wounds, and blurred vision. Recognising these signs can prompt earlier intervention and management of the condition, further reducing long-term health risks.
Read More
Concerns arise over rare eye condition linked to popular weight loss injections
Recent research indicates that individuals utilising semaglutide injections, commonly used for weight management and type 2 diabetes, have a quadrupled risk of developing a severe eye disorder compared to non-users. The medications in question, Ozempic and Wegovy, have been associated with an elevated risk of non-arteritic anterior ischemic optic neuropathy (NAION), a rare but potentially harmful eye condition.
Despite the concerning findings, the researchers involved have clarified that the overall incidence of the condition among users remains low, and definitive evidence that semaglutide is the direct cause of NAION is still lacking.
Produced by pharmaceutical giant Novo Nordisk, Wegovy is designed to promote significant weight loss. Clinical trials have shown that some individuals experience a reduction in body weight exceeding 10% after using the medication.
The popularity of these weight loss injections has surged recently, fueled in part by celebrity endorsements and public testimonials about their effectiveness in achieving rapid weight loss.
However, a rise in the unregulated online purchase of semaglutide injections has alarmed health professionals. The absence of proper checks on these internet-sourced medications raises serious concerns about their safety.
Further worries have been voiced over the misuse of semaglutide, with indications that the drug is increasingly being used for cosmetic weight loss, particularly to achieve a ‘beach-body’.
The common side effects associated with semaglutide include stomach pain, nausea, constipation, diarrhoea, and vomiting. Additionally, both Ozempic and Wegovy have been linked to potentially serious changes in vision, according to the latest studies.
NAION, which affects up to 10 in every 100,000 people, leads to vision loss due to diminished blood flow to the optic nerve and currently lacks an effective treatment.
Dr Joseph Rizzo, a leading researcher in the study, stated, “Our findings should be viewed as being significant but tentative, as future studies are needed to examine these questions in a much larger and more diverse population.”
A Novo Nordisk spokesperson responded to the findings by noting that NAION is not recognised as a known adverse drug reaction in the marketed formulations of semaglutide, which include Ozempic, Rybelsus, and Wegovy. They highlighted that semaglutide has been thoroughly examined in extensive real-world evidence studies and robust clinical development programmes.
Professor Graham McGeown from Queen’s University Belfast commented on the issue, emphasising the need for additional research given the sharp rise in semaglutide usage and its potential approval for uses beyond obesity and type 2 diabetes. “This issue deserves further study – but possible drug side-effects always need to be balanced against likely benefits,” he said.
Read More
Ozempic and other GLP-1 drugs show promise in reducing obesity-related cancer risks
In a significant medical discovery, a class of diabetes medications, including the widely-used drug Ozempic, has been linked to a decreased risk of numerous obesity-associated cancers. This revelation was detailed in a study published in the Journal of the American Medical Association (JAMA) on Friday, 5th of July, 2024.
The research meticulously analysed the health outcomes of Type 2 diabetes patients from 2005 to 2018, focusing on those treated with insulin compared to those administered GLP-1 agonists, such as Ozempic. The findings indicated a notable reduction in the risk of developing 10 out of 13 types of cancer examined in the study. The cancers showing decreased risk include those of the kidney, pancreas, oesophagus, ovaries, liver, and colorectum.
However, the study observed no substantial reduction in the risk of thyroid cancer and breast cancer among postmenopausal women. These findings underscore the complex relationship between metabolic disorders and cancer risks.
“Obesity is well known to be associated with at least 13 cancer types,” stated Rong Xu, the study’s lead author, in an email correspondence with AFP. Xu further commented, “Our study provides evidence that GLP-1RAs hold promise in breaking the link between obesity and cancer.”
The research not only highlights the efficacy of GLP-1 receptor agonists (GLP-1RAs) in managing diabetes but also their potential role in cancer prevention. The study encompassed several drugs within this category, including semaglutide, marketed as Ozempic, and liraglutide, among others, with Ozempic receiving approval in the United States in 2017.
GLP-1 agonists have been utilised for approximately two decades; however, a new generation of these drugs, including Ozempic, has gained popularity for their enhanced effects on weight loss.
The protective benefits observed might influence healthcare providers to favour GLP-1 treatments over other therapeutic options such as insulin for diabetes patients, as suggested by Xu. This shift could represent a pivotal evolution in the management of diabetes and its associated cancer risks, marking a significant stride forward in integrative disease prevention strategies.
Read More
Natural compound found in olives shown to lower blood sugar and aid weight loss, mouse study shows
A novel study conducted using mice models has highlighted the potential of elenolic acid, a natural compound extracted from olives, in mitigating obesity and type 2 diabetes. This groundbreaking research suggests that elenolic acid could serve as a basis for the development of affordable, safe natural products aimed at managing these prevalent health issues.
In a series of experiments, diabetic mice with obesity administered with elenolic acid orally displayed a significant reduction in body weight and enhanced glucose regulation within just one week. These results were noteworthy when compared to a control group of mice with obesity that did not receive the treatment. Remarkably, the glucose-lowering impact of elenolic acid was on par with liraglutide, an injectable diabetes medication, and surpassed the effectiveness of metformin, a commonly used oral diabetes drug.
Professor Dongmin Liu, the lead researcher and a professor at the Department of Human Nutrition, Foods and Exercise at Virginia Tech, explained the motivation behind their focus on natural compounds. “Lifestyle modifications and public health measures have had limited impact on the rising prevalence of obesity, one of the top risk factors for type 2 diabetes. Available obesity drugs are ineffective in weight loss maintenance, expensive and/or carry potential long-term safety risks. Our goal was to develop safer, cheaper and more convenient multi-targeting agents that can prevent the occurrence of metabolic disorders and type 2 diabetes,” stated Liu.
The research findings will be presented by Dr. Hana Alkhalidy, a scientist in Liu’s laboratory, at NUTRITION 2024, the premier annual event of the American Society for Nutrition.
The team at Virginia Tech has previously investigated various natural compounds targeting molecular aspects of metabolism in critical body parts like the pancreas, muscle, fat tissues, and liver. Their latest strategy focuses on stimulating hormone secretion in the gut, a method that could indirectly improve metabolic functions due to natural products’ generally poor bioavailability.
Their screening identified that elenolic acid, found abundantly in mature olives and extra virgin olive oil, stimulates the release of metabolic hormones GLP-1 and PYY in the gut. These hormones are integral during meals, enhancing satiety and regulating blood sugar and metabolism. The researchers synthesized elenolic acid from its precursor, oleuropein, which proved to be a cost-effective method compared to direct extraction from olives.
Further testing revealed that diabetic mice with obesity treated with elenolic acid for four to five weeks showed a 10.7% reduction in obesity and exhibited glucose levels and insulin sensitivity comparable to healthy, lean mice. Additionally, the treatment significantly curbed food intake and fostered weight loss, effects associated with increased levels of PYY and GLP-1 and decreased expression of agouti-related peptide, a hypothalamic peptide that promotes overeating and weight gain when overexpressed.
“Overall, the study showed that elenolic acid from olives has promising effects on hormone release and metabolic health, particularly in obese and diabetic conditions,” Liu remarked. He noted that the compound mimics the physiological conditions of eating to enhance gut metabolic hormone secretion, thereby helping to regulate energy balance and metabolic health.
Despite these promising results, the researchers cautioned that the concentration of elenolic acid in typical olive products is quite low, implying that the health benefits observed in the study are unlikely to be replicated through consumption of olives and olive oil alone.
The research team is now focused on elucidating the metabolic pathway of elenolic acid, from its absorption to its excretion. This exploration will provide further insights into the compound’s efficacy and safety, paving the way for potential clinical trials.
Read More
AI enhances efficiency of artificial pancreas, study confirms
Recent research conducted by the University of Virginia’s Center for Diabetes Technology reveals that incorporating artificial intelligence (AI) into an artificial pancreas system can significantly improve its operational efficiency. This innovative study marks a crucial advancement in the management of type 1 diabetes.
The study highlights that an AI-equipped artificial pancreas system is comparable in performance to a state-of-the-art experimental version in maintaining optimal blood glucose levels. The integration of AI not only matches the effectiveness of advanced systems but also offers potential applications in other medical devices that require minimal computational resources, like insulin pumps.
Dr Boris Kovatchev, the study’s lead author, emphasised the novelty of their approach, stating, “So far, this is the first clinical trial of a data-driven artificial pancreas system, which used an extensively trained neural network to deliver insulin automatically.” This system represents a significant shift towards more autonomous patient care in diabetes management.
The experimental setup involved 15 adult participants who used both the advanced artificial pancreas and the AI-enhanced system for 20 hours each. Results showed that the traditional advanced system kept blood sugar levels within the target range 87% of the time, closely followed by the AI-supported system at 86%.
Notably, the research demonstrated that the AI-supported pancreas system drastically cuts down the computational load by six times compared to traditional methods. “The AI-supported artificial pancreas is therefore more suitable for implementation in devices with low processing power, such as insulin pumps or pods,” the report noted, pointing towards a broader applicability in diabetes care technology.
Dr Kovatchev further explained the technical breakthroughs, saying, “Neural-net implementation allows the algorithm to learn from the data of the person wearing the system. This opens the door to real-time, AI-driven personalised insulin delivery.” This adaptation could lead to more tailored and effective diabetes management solutions for individuals.
The findings, published in the journal Diabetes Technology & Therapeutics, set a precedent for the future of diabetes care, highlighting the critical role of AI in enhancing the functionality and efficiency of medical devices aimed at chronic disease management.
Read More
Substantial rise in individuals at risk of type 2 diabetes in England, NHS reports
In a striking development reported by the NHS, the number of people in England identified as being at risk of developing type 2 diabetes has surged by over half a million in just one year. According to the latest data from the National Diabetes Audit, the figures for those diagnosed with non-diabetic hyperglycaemia, commonly referred to as pre-diabetes, rose from 3,065,825 in 2022 to 3,615,330 in 2023—an increase nearing 18%.
The increase is particularly pronounced among the younger population under the age of 40, witnessing a surge of almost 25% from 173,166 in 2022 to 216,440 in 2023. This early identification is pivotal as it allows the NHS to intervene sooner with diagnoses and preventive measures to halt the progression of the condition.
Individuals identified with non-diabetic hyperglycaemia exhibit elevated blood glucose levels that, although not high enough to warrant a diabetes diagnosis, significantly increase their risk of developing type 2 diabetes and cardiovascular diseases. This condition is often detected during routine blood tests at GP surgeries.
To counteract this trend, the NHS has implemented several innovative measures aimed at preventing type 2 diabetes and reducing obesity rates. This includes the internationally acclaimed Healthier You NHS Diabetes Prevention Programme, which, thus far, has enrolled over 1.6 million people. This nine-month intervention offers personalised support, focusing on healthy eating, lifestyle changes, enhanced physical activity, and weight management.
The implications of developing type 2 diabetes are severe and widespread, affecting not only the individual’s health but also placing a considerable strain on families and NHS resources. It is a leading cause of preventable sight loss among working-age individuals and contributes significantly to kidney failure, lower limb amputation, and an increased risk of heart attacks, strokes, and certain types of cancer.
NHS Chief Executive, Amanda Pritchard, highlighted the critical nature of these findings, stating, “These figures are concerning but they show exactly why the NHS is taking radical action to stem the tide of rising levels of obesity and type 2 diabetes – through our world first prevention programme and our soup and shakes diets. Type 2 diabetes is a growing problem for patients and not only is it linked to kidney failure, amputation, heart attack, stroke and many of the common types of cancer, it also adds pressure to NHS services. Doing nothing is not an option for the NHS, so we will continue to develop services that support people at risk of developing type 2 diabetes to lead healthier lives. If you are worried about developing the condition, please do come forward and get the help you need.”
In England, approximately 90% of individuals with diabetes have type 2. The risk factors are diverse, encompassing genetics, ethnicity, and lifestyle factors such as obesity.
Moreover, the NHS has dedicated £14.5 million to support up to 140,000 young individuals aged 18 to 39 with additional tailored health checks and diabetes management support. This initiative, dubbed ‘T2Day: Type 2 Diabetes and the Young’, offers enhanced one-to-one reviews and access to innovative treatments to better manage their condition and prevent complications.
Dr Clare Hambling, National Clinical Director of Diabetes and Obesity at NHS England, remarked, “Type 2 diabetes in people under 40 is a growing problem globally – England is no exception, meaning there is an ever-increasing challenge for the NHS – which is why we developed this world-first targeted support for these high-risk people living with diabetes.”
Additionally, a new expansion of the NHS Type 2 Diabetes Path to Remission Programme aims to help more than 10,000 individuals with type 2 diabetes and obesity to lose weight and improve their health. This national programme is set to double its capacity this year, building on the success of over 23,000 people who have already participated since its inception in 2020.
The NHS in England currently allocates approximately £10 billion annually, about 10% of its total budget, to manage diabetes. This figure complements the £6.5 billion spent annually on obesity treatments. Following the disruptions caused by the COVID-19 pandemic, NHS England has also provided £36 million to help local teams restore diabetes services to pre-pandemic levels.
The NHS Long Term Plan continues to outline crucial strategies aimed at reducing disparities in service access and improving the quality of treatment and outcomes for individuals living with diabetes, reinforcing the commitment to combat this escalating health challenge.
Read More
Oral semaglutide proven effective in managing type 2 diabetes and enhancing cardiovascular health
A meticulous study recently published in the Journal of Clinical Medicine has delved into the impact of oral semaglutide on patients with type 2 diabetes (T2D), highlighting its dual benefits on glycaemic control and cardiovascular wellness.
Semaglutide, distinguished as the inaugural oral anti-diabetic treatment specifically for T2D, functions as a glucagon-like peptide-1 receptor agonist (GLP-1RA). It has been proven to regulate glycaemic levels and reduce body weight (BW). Its safety and effectiveness have been corroborated through numerous clinical trials.
The extensive PIONEER programme assessed the efficacy of oral semaglutide across various stages of diabetes, involving treatment modalities that ranged from monotherapy to combination therapies with other oral glucose-lowering agents. Following the promising outcomes of this programme, the United States Food and Drug Administration (FDA) endorsed the drug in 2019, with subsequent approval by the European Medicines Agency (EMA) in 2020.
Guidelines in both America and Europe recommend oral semaglutide for T2D patients, especially those at high or very high risk of cardiovascular diseases (CVD), irrespective of their glycated haemoglobin (HbA1c) levels. This recommendation underscores the drug’s cardiovascular benefits.
However, the findings from the PIONEER study, though promising, call for further large-scale studies to conclusively determine the drug’s capability in reducing CVD risks. Additionally, the readiness of healthcare providers to incorporate this medication into everyday clinical practice warrants further evaluation.
The current retrospective study took place at two university-based diabetes centres in Italy, utilising data from an electronic chart system software designed for managing medical records in Italian diabetes outpatient clinics. This system recorded comprehensive patient data, including BW, HbA1c levels, waist circumference, serum creatinine, blood glucose levels, blood pressure, lipid profiles, aspartate aminotransferase (AST), estimated glomerular filtration rate (eGFR), among other laboratory results, as well as concurrent medications.
Patients received oral semaglutide during clinic visits, starting with a three mg dose, subsequently increased to seven mg, and in some cases, elevated to 14 mg to further enhance glycaemic control. These adjustments occurred over a monitoring period of up to six months.
The clinical improvements were notable in patients with recently diagnosed diabetes who showed significant enhancements in HbA1c levels and reductions in BW within six months of treatment initiation.
The study involved 192 Caucasian participants, predominantly around 67 years of age, with 44% being female and an average diabetes duration of nine years. Median fasting glucose and HbA1c levels stood at 146 mg/dL and 7.9%, respectively.
Prior to their oral semaglutide regimen, participants were treated with various medications, including sodium-glucose cotransporter-2 inhibitors (SGLT2i), basal or fast-acting insulin, other GLP-1RAs, pioglitazone, metformin, DPP4 inhibitors, or sulfonylureas. During the six-month treatment phase with oral semaglutide, most patients were administered a seven mg dose, with only 2% receiving the 14 mg dose.
The study revealed no significant differences in HbA1c reduction between genders, but all participants experienced comparable weight loss. Significant improvements were also recorded in lipid profiles, waist circumference, blood pressure, and microalbuminuria levels after six months of treatment, underscoring oral semaglutide’s comprehensive benefits in metabolic health and CVD risk reduction.
In summary, oral semaglutide not only maintained optimal glycaemic control and facilitated weight reduction but also enhanced cardiovascular risk factors, including lipid profiles and blood pressure levels. The clinical relevance of oral semaglutide was evident even at a minimal dosage of seven mg, particularly among newly diagnosed patients, and the drug was well-tolerated even at the higher 14 mg dosage.
Read More
How Continuous Glucose Monitors (CGMs) are changing the fight against obesity
Continuous Glucose Monitors (CGMs), initially developed for diabetes management, are gaining recognition for their role in aiding individuals with obesity, especially those at risk of developing diabetes. With these devices soon to be available over-the-counter in the United States, there is a new frontier in proactive health monitoring.
Lori Wenz, a nurse practitioner at Western Colorado Weight Care in Grand Junction, Colorado, discussed the expanding use of CGMs beyond their traditional scope during her presentation at the 2024 Obesity Medicine Association conference. She emphasised that CGMs not only enhance patient motivation by improving awareness of how diet and activity impact metabolic health but also play a crucial role in adherence to nutritional guidance and pharmacotherapy.
A significant proportion of the American adult population remains unaware of their pre-diabetic or diabetic status. According to the Centers for Disease Control and Prevention, approximately 38% of adults have pre-diabetes, of which up to 80% are unaware. Additionally, around 23% of the 11.6% of Americans diagnosed with diabetes are also ignorant of their condition. Notably, up to 90% of those diagnosed with diabetes have either overweight or obesity, highlighting the intertwined nature of obesity and diabetes.
The off-label use of CGMs in obesity management is gaining acceptance as both clinicians and patients become increasingly proactive in monitoring potential diabetes risks and overall health. Wenz reported a significant increase in the off-label application of CGMs over the past three to five years, attributed largely to technological advancements that have reduced costs and enhanced device integration with mobile technology.
CGMs are particularly useful in diagnosing pre-diabetes and managing glucose levels to delay or even reverse the progression to diabetes. The devices provide real-time glucose readings, revealing the impact of lifestyle choices on glucose fluctuations, which can be a revelation for many users. This encourages more informed decisions about diet and exercise, leading to better health outcomes.
In a significant development, the FDA recently approved the Dexcom Stelo Glucose Biosensor System, the first over-the-counter CGM, for individuals over 18 who are not on insulin therapy. This device, which provides glucose measurements every 15 minutes and can be worn for up to 15 days, represents a major step forward in making glucose monitoring more accessible.
Despite the advantages, the use of CGMs in non-diabetic patients presents unique challenges. There are no established glucose norms for individuals without diabetes, and interpreting CGM data can be complicated. Moreover, alarms designed for diabetic users can be bothersome for those without the condition, potentially disrupting sleep and causing undue stress.
Alaina Vidmar, MD, at the Keck School of Medicine of the University of Southern California, discussed the benefits of CGMs in paediatric obesity interventions. Real-time glucose data helps educate young patients about their body’s reactions to different foods and reinforces adherence to dietary restrictions, which is crucial for effective weight management and prevention of diabetes.
The advent of over-the-counter CGMs is poised to transform the landscape of obesity management and diabetes prevention. As the market expands and prices become more competitive, these devices offer a promising tool for individuals to take control of their health, potentially averting the progression to diabetes and improving overall metabolic health. The holistic integration of CGMs with innovative health strategies, pharmacotherapy, and even surgery holds the promise of enhancing life quality and longevity for individuals with obesity.
Read More
European regulators find no evidence of link between new obesity medication and suicidal thoughts
Following an extensive nine-month investigation, European medical regulators have concluded that there is no evidence to suggest that GLP-1 receptor agonists, such as Ozempic and Wegovy, contribute to suicidal ideation or behaviours. This conclusion by the European Medicines Agency (EMA) aligns with a similar assessment conducted by the U.S. Food and Drug Administration (FDA) earlier in January, which also found no causal connection between these widely used medications for weight loss and diabetes and the risk of suicidal thoughts.
The investigation by the EMA began in July, 2023, after anecdotal instances were reported where patients exhibited self-harm thoughts while being treated with GLP-1 receptor agonists, specifically liraglutide (marketed as Saxenda by Novo Nordisk) and semaglutide (known commercially as Ozempic and Wegovy, also by Novo Nordisk). The concern prompted the EMA’s Pharmacovigilance Risk Assessment Committee to demand further information from the manufacturers of these medications in November.
Throughout the investigation, the committee meticulously analysed various sources including medical records, clinical trial data, post-marketing surveillance reports, and other academic studies. Notably, a study published in Nature Medicine indicated that the risk of suicidal ideation was actually lower in patients using GLP-1 drugs compared to those treated with other medications for obesity and diabetes. Ultimately, the EMA committee concluded that the evidence does not support a causal link between the use of GLP-1 receptor agonists and increased suicidal risk.
Despite these findings, the EMA has mandated continuous monitoring by manufacturers of GLP-1 based medications for any future incidents of suicidal thoughts or actions. This ongoing vigilance reflects a cautious approach, particularly given the historical context where earlier obesity treatments, such as rimonabant, were withdrawn from the European market in 2008 due to their association with increased suicidal ideation risks.
GLP-1 based treatments, including Ozempic, Wegovy, Eli Lilly’s Mounjaro, and Zepbound, have seen a surge in popularity recently. However, this increase in usage has coincided with sporadic anecdotal reports linking the drugs to suicidal thoughts, thus prompting these detailed investigations.
The FDA, in its preliminary review statement in January, mentioned that while a definitive exclusion of any risk is challenging, it is committed to further investigation to clarify this potential link. It is important to note that while the FDA’s approvals for Wegovy and Zepbound for obesity management include advisories for physicians to monitor for signs of suicidal thoughts, similar advisories are not included on the labels of Ozempic and Mounjaro, which are approved for managing type 2 diabetes.
This comprehensive review by regulatory bodies underscores a significant step in ensuring the safety and efficacy of GLP-1 medications, reaffirming their use in clinical practice amidst growing concerns over possible psychiatric side effects.
Read More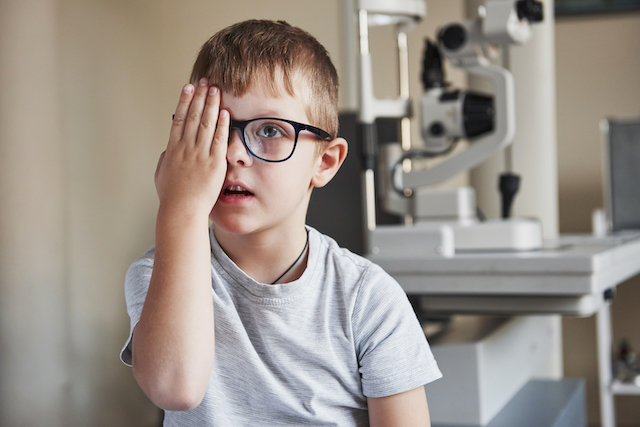
AI breakthrough improves eye exam rates in youth with diabetes
In a ground-breaking study conducted by the Johns Hopkins Children’s Center, researchers have demonstrated a significant leap forward in the field of diabetic eye care through the implementation of autonomous artificial intelligence (AI) for eye examinations. This innovative approach has markedly improved the rate of screening completions among children and adolescents with diabetes, thereby offering a promising avenue to combat the incidence of diabetes-related eye diseases (DED), which can lead to blindness if left unchecked.
The study, which has been a focal point of attention in a recent Johns Hopkins news release, utilises a non-intrusive method whereby images of the retina are captured without the necessity for pupil dilation. Following this, AI technology analyses the images to provide instantaneous results, distinguishing this method from traditional screening procedures which often require an additional appointment and dilation of the eyes.
The significance of this research cannot be overstated, especially considering its potential to bridge healthcare disparities. Historically, minority and economically disadvantaged youth, who are at a heightened risk of developing DED, have faced substantial barriers in accessing regular eye screenings. The AI-driven method heralded by this study not only promises to close these care gaps but also to enhance adherence to screening protocols among these populations.
Published in the esteemed journal Nature Communications, the study analysed eye exam completion rates among individuals under 21 years of age suffering from type 1 and type 2 diabetes. Remarkably, it was found that all participants who underwent the AI-based screenings completed their eye assessments, a stark contrast to traditionally lower adherence rates.
Diabetic retinopathy, a condition affecting 4% to 9% of youth with type 1 diabetes and 4% to 15% of those with type 2 diabetes, underscores the urgency for regular screenings. The American Diabetes Association estimates that approximately 238,000 individuals under the age of 20 are living with diagnosed diabetes, making early detection and treatment of eye conditions critical to preventing the advancement of DED.
Despite the general recommendation for annual screenings, traditional methods have seen a participation rate of only 35% to 72% among young diabetic patients, with even lower rates observed in minority and economically disadvantaged groups. Barriers such as confusion over the necessity of screenings, inconvenience, and lack of accessibility have all contributed to this shortfall.
The Johns Hopkins study introduced a novel solution to these challenges by incorporating autonomous AI screening into routine visits to the endocrinologist, thereby eliminating the need for separate appointments and the discomfort of eye dilation. This method, which involves taking four images of the eye to assess for diabetic retinopathy, has not only streamlined the screening process but also facilitated immediate follow-up actions when necessary.
This research initiative enrolled 164 participants from the Johns Hopkins Pediatric Diabetes Center, with a demographic makeup that was both gender and ethnically diverse. The findings revealed a 100% completion rate for eye exams among the group subjected to AI screenings, a significant improvement over traditional methods.
The study’s lead, Dr. Risa Wolf, emphasised the dual benefits of this approach: increased screening rates and the potential to enhance health equity. By making screenings more accessible and convenient, the researchers hope to prevent the progression of diabetic eye disease across all demographics.
However, it is important to note the study’s limitations, including the current FDA approval status of the autonomous AI for individuals under 21 and the potential bias due to some participants’ prior familiarity with AI screenings from a previous study.
Funded by the National Eye Institute of the National Institutes of Health and the Diabetes Research Connection, this study represents a pivotal step forward in diabetic eye care. It not only underscores the transformative potential of AI in healthcare but also highlights the critical need for innovative solutions to improve access and outcomes for vulnerable populations.
Read More
FDA issues alert on counterfeit semaglutide products in the U.S.
The U.S. Food and Drug Administration (FDA) has recently issued a crucial warning to adults with diabetes in the United States about the presence of counterfeit semaglutide in the country’s drug supply chain. This alert comes following an ongoing FDA investigation into the distribution of fake versions of the 1 mg subcutaneous semaglutide, known commercially as Ozempic and manufactured by Novo Nordisk.
The FDA’s investigation has led to the seizure of thousands of units of these counterfeit products. Key identifiers of the fake medication include lot number NAR0074 and serial number 430834149057. These specific batches have been confirmed as counterfeit and are advised not to be used.
A further cause for concern highlighted by the FDA is the discovery of counterfeit needles accompanying the medication. The sterility of these needles cannot be assured, posing a heightened risk of infection for users. Additional counterfeit components identified by the FDA include the pen label, health care professional and patient information leaflets, and the packaging box.
The FDA is urging wholesalers, retail pharmacies, healthcare providers, and patients to diligently check their semaglutide products’ lot and serial numbers. While the FDA, in partnership with Novo Nordisk, is currently conducting tests on the seized counterfeit products, there is yet no comprehensive information about the content, quality, or safety of these fakes.
To date, the FDA has received reports of five adverse events associated with the use of these counterfeit semaglutide products. These incidents align with the typical side effects of authentic semaglutide, and thankfully, none of the reported cases have been serious. The FDA encourages reporting of any adverse events through its MedWatch Safety Information and Adverse Event Reporting Program, either via online submission or fax at (1-800) FDA-0178.
The FDA advises pharmacies to source genuine semaglutide only through Novo Nordisk’s approved distributors. Patients should obtain the drug strictly with a valid prescription from state-licensed pharmacies and are advised to inspect the product thoroughly for any signs of counterfeiting before use. Any suspicions or discoveries of counterfeit products should be promptly reported to the FDA. This can be done by calling the local FDA consumer complaint coordinator or by reporting directly via the FDA’s official website.
Read More
Novo Nordisk’s $2.3 billion French investment to enhance obesity drug output
Novo Nordisk has declared a substantial $2.3 billion investment aimed at amplifying the output of its highly sought-after obesity and diabetes medications at its Chartres facility in France, in a move to satiate the escalating demand. This financial injection will notably enhance the manufacturing capabilities for existing products such as Ozempic and Wegovy, alongside other burgeoning obesity treatments, according to the Danish pharmaceutical giant.
Europe is currently grappling with a supply crisis of the diabetes medication Ozempic, which shares the active ingredient semaglutide with the widely acclaimed weight management drug Wegovy—yet to be broadly distributed across Europe.
In response to the off-label consumption of Ozempic, Novo Nordisk has imposed restrictions within the European Union. Concurrently, Germany is considering export prohibitions, while Belgium has already enacted a ban on prescribing the weekly injection for non-diabetes purposes.
Despite efforts by the UK government to restrict the use of Ozempic to non-weight loss purposes in July, a Reuters investigation discovered the drug is still being acquired by individuals without diabetes for weight management.
This announcement follows Novo Nordisk’s recent proclamation of a $6 billion expenditure in Denmark to augment production capabilities. Additionally, this venture represents a significant endorsement for French President Emmanuel Macron’s economic strategies amidst a looming global downturn, aiming to sustain the momentum in reducing French unemployment figures.
President Macron had advocated for this investment during his “Choose France” summit, which reportedly persuaded Novo Nordisk’s CEO Lars Fruergaard Jorgensen to commit to the expansion. The investment also echoes Eli Lilly’s recent decision to construct a $2.5 billion manufacturing plant in Germany, similarly motivated by heightened demand for diabetes and obesity treatments.
Analysts predict the obesity drug market could reach a staggering $100 billion by 2030. Novo Nordisk’s French investment will notably expand its capacity for intricate manufacturing processes, specifically the intricate filling of injection pens with semaglutide, and the subsequent assembly and packaging of these pens.
Though details were scant earlier this month regarding the augmentation of in-house production for Ozempic and Wegovy’s European variant, Novo Nordisk has confirmed that the Chartres expansion has commenced, with completion slated between 2026 and 2028, promising the creation of 500 new job opportunities, adding to the near 2,000-strong workforce currently employed at the factory.
Read More