
Novo Nordisk’s $2.3 billion French investment to enhance obesity drug output
Novo Nordisk has declared a substantial $2.3 billion investment aimed at amplifying the output of its highly sought-after obesity and diabetes medications at its Chartres facility in France, in a move to satiate the escalating demand. This financial injection will notably enhance the manufacturing capabilities for existing products such as Ozempic and Wegovy, alongside other burgeoning obesity treatments, according to the Danish pharmaceutical giant.
Europe is currently grappling with a supply crisis of the diabetes medication Ozempic, which shares the active ingredient semaglutide with the widely acclaimed weight management drug Wegovy—yet to be broadly distributed across Europe.
In response to the off-label consumption of Ozempic, Novo Nordisk has imposed restrictions within the European Union. Concurrently, Germany is considering export prohibitions, while Belgium has already enacted a ban on prescribing the weekly injection for non-diabetes purposes.
Despite efforts by the UK government to restrict the use of Ozempic to non-weight loss purposes in July, a Reuters investigation discovered the drug is still being acquired by individuals without diabetes for weight management.
This announcement follows Novo Nordisk’s recent proclamation of a $6 billion expenditure in Denmark to augment production capabilities. Additionally, this venture represents a significant endorsement for French President Emmanuel Macron’s economic strategies amidst a looming global downturn, aiming to sustain the momentum in reducing French unemployment figures.
President Macron had advocated for this investment during his “Choose France” summit, which reportedly persuaded Novo Nordisk’s CEO Lars Fruergaard Jorgensen to commit to the expansion. The investment also echoes Eli Lilly’s recent decision to construct a $2.5 billion manufacturing plant in Germany, similarly motivated by heightened demand for diabetes and obesity treatments.
Analysts predict the obesity drug market could reach a staggering $100 billion by 2030. Novo Nordisk’s French investment will notably expand its capacity for intricate manufacturing processes, specifically the intricate filling of injection pens with semaglutide, and the subsequent assembly and packaging of these pens.
Though details were scant earlier this month regarding the augmentation of in-house production for Ozempic and Wegovy’s European variant, Novo Nordisk has confirmed that the Chartres expansion has commenced, with completion slated between 2026 and 2028, promising the creation of 500 new job opportunities, adding to the near 2,000-strong workforce currently employed at the factory.
Read More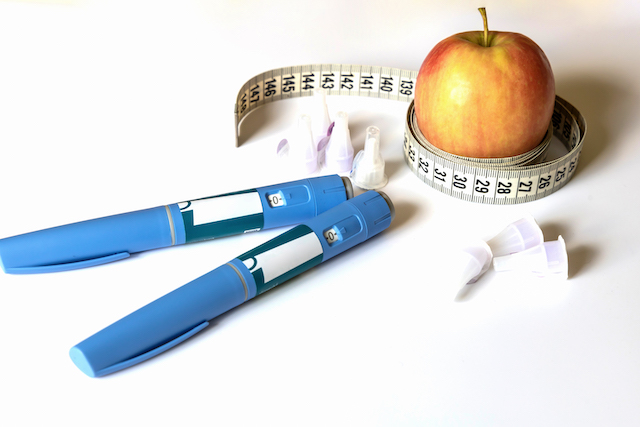
The limited impact of Ozempic on the U.S. obesity epidemic
The term ‘obesity’ elicits a range of interpretations. Some view it as merely another way to describe excess weight, while others perceive it as a derogatory label for larger body sizes. Still, some consider it a reflection of personal failings, such as a lack of discipline or willpower. However, for over a decade, the medical field has acknowledged obesity as a chronic health condition, akin to diseases like cancer, diabetes, and hypertension. This disease significantly elevates the risk of severe COVID-19 outcomes, is connected to numerous health complications, and is responsible for approximately 4 million preventable deaths annually. Moreover, obesity manifests in various forms, with diverse origins, clinical signs, and treatment responses.
The surge in popularity of GLP-1 medications such as Ozempic, Wegovy, and Mounjaro has somewhat simplified this complex issue. These drugs are often hailed as the ultimate solution to obesity, a perspective that overlooks the multifaceted nature of the condition. Unfortunately, Ozempic alone cannot address America’s obesity crisis. Obesity extends beyond mere physical inactivity or excessive eating. It’s influenced by a range of factors including genetic predispositions, mental health, socio-economic conditions, and environmental factors.
In clinical settings, the variation in obesity cases is significant. For instance, a mutation in the MC4R gene is associated with an 18% increased likelihood of obesity, while certain antipsychotic medications can lead to substantial weight gain. Although GLP-1 medications can be beneficial, they primarily address hormonal imbalances and do not tackle other contributing factors. This reductionist approach is also evident in the use of Body Mass Index (BMI) to diagnose obesity. BMI, initially designed for white European males, often inaccurately represents obesity levels in different ethnic groups, leading the American Medical Association to advise against its sole use. Currently, a global commission of experts is redefining obesity, moving away from height and weight measurements to focus on specific symptoms and signs.
The response to treatment among patients with obesity also varies greatly. For example, the GLP-1 drug Wegovy showed an average body weight reduction of 16% in a study, yet individual results ranged widely. This underscores the need for personalised treatment plans rather than a singular drug-based approach. However, the U.S. healthcare system faces significant challenges in this regard. With only a small number of physicians specialised in obesity treatment and federal restrictions on covering obesity medications, only a fraction of those who could benefit from such treatments receive them. Instead, many are advised to simply eat less and exercise more, a strategy that overlooks the complexity of obesity.
Effective obesity treatment involves a multidisciplinary approach, combining diet, exercise, behavioural therapy, medication, and sometimes surgery. Unfortunately, the scarcity of specialised physicians and the prevalence of misleading diet products and scams exacerbate the issue. The U.S. weight loss market, valued at $160 billion in 2023, is a testament to this. Moreover, misconceptions about GLP-1 medications, such as the idea that they are a cure-all for obesity, lead to unrealistic expectations and criticisms. Like insulin or hypertension treatments, discontinuing GLP-1 drugs can result in a reversal of their effects, a fact that should be recognised rather than criticised.
Addressing obesity, which costs the U.S. around $1.7 trillion annually, requires acknowledging the progress made with GLP-1 drugs while also understanding their limitations. A holistic, patient-centred, and empathetic approach to obesity treatment is essential. This approach should not only address the unique needs and circumstances of each individual but also aim to improve overall health and well-being. While medications like Ozempic, Wegovy, and Mounjaro offer significant potential, they are not the all-encompassing solution often portrayed in the media. A broader, more nuanced understanding and response to obesity is crucial for effective management and treatment.
Read More
AstraZeneca makes big push into obesity treatment with new pill partnership
AstraZeneca, the United Kingdom’s pharmaceutical giant, has entered a strategic partnership with Eccogene, a Shanghai-based biotech firm, to co-develop a groundbreaking pill designed to combat obesity and type 2 diabetes.
This alliance marks AstraZeneca’s significant foray into the burgeoning sector of weight management medications, underpinned by an exclusive licensing contract focusing on an investigational drug, ECC5004. The said compound is touted to address not only obesity but also a spectrum of cardiometabolic disorders, including heart disease and stroke, ailments afflicting over a billion people worldwide.
Eccogene is poised to receive payments that could sum up to a substantial $2 billion, which is approximately £1.6 billion, as per the agreed terms.
ECC5004 is currently undergoing phase 1 trials, with AstraZeneca setting its sights on advancing to phase 2 clinical evaluations by the subsequent year’s end. Additionally, the pharma titan is nurturing two other nascent-stage injectable obesity therapies.
The innovative ECC5004, if it passes clinical muster, is envisioned to be administered orally once daily, a standalone treatment or potentially in conjunction with other drugs targeting various cardiometabolic diseases. This positions it distinctively against the prevailing injectables that are typically administered weekly.
Operating as a GLP-1 agonist, ECC5004 is designed to replicate the function of the GLP-1 hormone, which is naturally secreted post-food intake.
Pascal Soriot, AstraZeneca’s CEO, highlighted the critical demand for effective obesity interventions across Western nations, Latin America, and South Asia, where abdominal obesity is rampant, precipitating heightened risks of hypertension and diabetes.
Soriot indicated that while the journey to market might span several years, ECC5004 could potentially be more economically accessible than existing options. Due to its simplified chemical structure that permits cheaper production costs, the drug could cater to a wider demographic, including those in lower-income nations where AstraZeneca maintains a robust footprint.
As the competition intensifies in the international market for obesity drugs, demand has surged for Novo Nordisk’s Wegovy and Ozempic, prompting supply challenges. With Wegovy’s pricing set at £73.25 per pack monthly on the NHS and reaching £199 at retail pharmacies, its sales and profits have climbed sharply, elevating Novo Nordisk to be Europe’s highest-valued company by market capitalisation.
Notably, Eli Lilly’s Mounjaro has demonstrated superior weight loss outcomes compared to Wegovy and recently secured approvals for weight management in the UK and US. Market analysts from UBS have predicted that Mounjaro could emerge as one of the most successful pharmaceuticals ever, with projected peak sales around £20 billion.
Pharmaceutical titans Novo Nordisk, Eli Lilly, and Pfizer are all in the race to create oral anti-obesity medications, which promise cost-effectiveness and ease of administration over injections.
Bolstered by its oncology drugs and the diabetes treatment Forxiga, AstraZeneca has reported a 5% revenue increase, totaling $33.8 billion in the year’s first three quarters. The firm also lifted its revenue and profit forecasts for the full year, announcing approvals for additional cancer treatments.
AstraZeneca’s COVID-19 vaccine, crafted in collaboration with Oxford University, was pivotal during the pandemic, credited with saving over 6 million lives globally within its inaugural year as per independent assessments.
However, AstraZeneca currently faces two high court cases in London related to the vaccine’s side effects. The company is expected to contest these allegations.
The World Health Organization last year affirmed the vaccine’s safety and efficacy for individuals 18 years and older, labelling TTS occurrences as exceptionally rare and characteristically presenting severe blood clots.
Read More
Pfizer aims to enter the obesity treatment arena with danuglipron, a novel GLP-1 targeting pill
In the competitive landscape of obesity pharmacotherapy, Pfizer is on the cusp of revealing pivotal trial data for its investigational drug danuglipron. This oral medication, administered twice daily, is poised to challenge the market dominance of prominent weight-loss therapies Wegovy and Mounjaro.
Danuglipron operates by influencing the glucagon-like peptide-1 (GLP-1) receptor, which has recently revolutionised the pharmaceutical industry, resulting in substantial economic shifts within the stock market. Through its strategic targeting of this receptor, the drug aims to become a cornerstone in the management of obesity.
Pfizer’s commitment to this endeavour is evident through the initiation of a rigorous Phase 2 trial, designed to thoroughly evaluate danuglipron’s ability to achieve significant weight reduction in individuals with obesity. The financial community, particularly Leerink Partners’ analyst David Risinger, anticipates a full disclosure of the study outcomes potentially by October 31.
For Pfizer, the urgency to diversify its product portfolio has never been greater. The pharmaceutical giant has faced a downturn in its COVID-19 vaccine and therapeutic product demand, compelling a downward revision of its revenue projections. This decline has led to a notable 40% dip in Pfizer’s stock value since the beginning of the year.
The strategic importance of danuglipron has been amplified following Pfizer’s decision in June to discontinue another candidate within its GLP-1 based weight-loss pipeline. The discontinuation was a setback, sharpening the focus on danuglipron as a critical asset in the company’s quest to secure a competitive position in the burgeoning GLP-1 market segment.
As Pfizer prepares to release its findings, the pharmaceutical, obesity care, and weight management industries are watching closely. Danuglipron not only carries the potential to alter the obesity treatment paradigm but also represents a vital opportunity for Pfizer to demonstrate resilience and innovation in the face of shifting healthcare needs. The success of this drug is particularly crucial as Pfizer measures itself against Eli Lilly’s promising GLP-1 oral therapy, which is also vying for a share of this lucrative market.
Read MoreDigital tool for specialist weight management services shows promising results
In a groundbreaking investigation led by the team at University Hospitals Coventry and Warwickshire NHS Trust (UHCW), the potential and efficacy of digital platforms tailored for advanced weight management have been highlighted.
The research revolved around assessing the eagerness, acceptance, and active participation of patients on standby for their first-ever specialist weight management consultation. In the United Kingdom, specialised weight management services, often referred to as tier 3 services, offer a holistic approach to tackling obesity. These specialised services are generally anchored in hospitals or clinic facilities and bring together a diverse group of healthcare specialists. This includes dietitians, psychologists, specialist nurses, and doctors, all proficient in the realm of weight management.
For the purposes of this research, an NHS-approved digital platform named Gro Health was integrated into the service offering. This avant-garde health application propels numerous healthcare routes, with its tier 3 weight management feature, “W8Buddy”, acting as an online weight loss clinic. This feature delivers structured learning sessions, both individual and group coaching, an expansive list of over 2,000 recipes and meal schedules, and tools for health and nutrition tracking to chart progress.
The study drew in 199 prospective patients eagerly waiting for their appointment at the NHS Trust’s tier 3 weight management service.
Preliminary results indicate that over half of these individuals expressed genuine interest in the application. An impressive one-third went on to actively engage with the digital platform, highlighting the immense potential of such digital interventions in the specialised weight management scenario.
The engagement analysis unearthed intriguing data points. Those prone to emotional eating or those with an escalated BMI exhibited an increased propensity towards the Gro Health application. Meanwhile, aspects like age, ethnic background, and metabolic indicators like glycemia and lipid readings did not notably sway the interest.
These findings could serve as a blueprint for revolutionising weight management strategy. As digital healthcare tools evolve and gain traction, they stand poised as formidable and expansive strategies to confront the global issue of obesity.
Charlotte Summers, a behavioural change expert and the Founding Chief Operations Officer, expressed her enthusiasm, noting, “The pronounced interest demonstrated by patients in the Gro Health W8Buddy tool for weight management is truly heartening.”
She drew attention to the evident link between emotional eating, a raised BMI, and heightened engagement, highlighting, “This relationship underscores the transformative capacity of precise digital strategies in addressing weight-related concerns.”
Summers further elaborated on the journey ahead, “As we venture into providing tier 3 and 4 weight management services, we’re thrilled about tailoring these platforms with firsthand insights from both patients and healthcare providers. Such a collaborative effort not only champions a patient-driven model but also deepens our grasp on their preferences and anticipations. This, in turn, empowers us to offer top-tier, accurate care, be it through enhancing conventional healthcare avenues or pioneering virtual healthcare experiences.”
The study’s authors stress the need for continued exploration into understanding the challenges and motivators behind adopting digital tools and emphasise the importance of rigorously assessing their impact within specialised weight management services.
The rise of digital health platforms is sculpting the future of healthcare. This specific investigation underscores the transformative power of such tools, all while highlighting the necessity to unravel the complexities of patient engagement. As we witness the proliferation and capabilities of digital health platforms, the persistent quest to maximise their utility for patients and the broader healthcare spectrum is paramount.
Stay tuned for more revelations as ongoing studies continue to sculpt this rapidly evolving domain of weight management.
Read More
Weight-loss medication Wegovy to be prescribed by NHS amid limited availability
In the UK, the NHS (National Health Service) in England is gearing up to administer the weight-loss drug Wegovy, also known by its scientific name semaglutide, under a “controlled and limited launch.” This initiative, starting from September 4, 2023, will operate via specialist NHS weight management services, where the drug will be prescribed in conjunction with a regimen involving a reduced-calorie diet and physical exercise. The patients targeted in this program must have a Body Mass Index (BMI) exceeding 30 and at least one weight-related health issue to qualify.
The drug, produced by Danish pharmaceutical company Novo Nordisk, received approval for NHS usage earlier in 2023, a sanction granted by the National Institute for Care and Excellence (NICE), which has recommended its usage be capped at a two-year period.
Addressing the prospects of this new treatment, UK Prime Minister Rishi Sunak heralded the introduction of Wegovy as a potential “game-changer” in the battle against obesity, a condition known to predispose individuals to serious health complications such as hypertension, diabetes, and various forms of cancer. The prime minister expressed optimism that this strategy would alleviate the strain on NHS resources, contribute to the reduction of waiting lists, and foster improved health and longevity among the populace.
Echoing these sentiments, Novo Nordisk anticipates that the drug will enhance the range of options available for individuals grappling with obesity, thus facilitating their journey towards achieving healthier body weights.
Earlier in June, the government had set aside £40 million for a pilot project intended to widen the accessibility of weight-loss injections as part of a robust strategy to curb obesity.
However, the initiative encountered a significant hurdle as Novo Nordisk reported an impending shortage in the supply of semaglutide, a situation anticipated to persist for an unspecified period. Despite this, the company reassured that a “proportion of available supply” would be designated for NHS services, with a firm commitment to prioritising patients demonstrating the “highest unmet medical need.”
An official communication from the NHS noted that in line with the guidance from NICE, measures are underway to inaugurate weight management undertakings, while also making efforts to restore the drug supply, particularly for individuals diagnosed with type 2 diabetes.
According to NHS projections, approximately 50,000 qualified patients in England stand to benefit from Wegovy, provided through NHS specialist weight management facilities capable of offering the necessary multi-disciplinary care.
Backing the efficacy of Wegovy, Novo Nordisk presented findings from a comprehensive five-year research project titled the Select trial. The study, which incorporated 17,604 adults aged 45 and above from 41 different countries, revealed that the drug could diminish the likelihood of heart attacks or strokes in individuals with obesity harbouring cardiovascular diseases by a considerable twenty percent. Participants in this trial were characterised by a BMI exceeding 27, established cardiovascular ailments, and devoid of any diabetes history.
Read More
Novo Nordisk’s weight-loss drug Wegovy demonstrates heart benefits in latest trial
Novo Nordisk’s groundbreaking obesity drug, Wegovy, has been shown to offer significant cardiovascular advantages, according to the results of a major late-stage trial announced on Tuesday (8th of August, 2023). This revelation not only highlights the efficacy of the medication but also helps in reshaping its perception beyond merely being a lifestyle drug.
The clinical study, named SELECT, revealed that individuals treated with Wegovy experienced a 20% reduction in the occurrence of heart attack, stroke, or death from heart-related diseases, in comparison to those who were administered a placebo. These findings far exceed the 15-17% reduction that had been anticipated by investors and analysts, although it’s worth noting that the results have not yet been subject to peer review.
Involving a substantial cohort of 17,500 participants, the SELECT trial specifically targeted individuals with overweight or obesity aged 45 or older, with a history of heart disease, but without prior diagnosis of diabetes. The trial, which spanned nearly five years, aimed to determine whether Wegovy’s weekly injection could confer tangible medical advantages.
The announcement of these positive results led to a surge in Novo Nordisk’s shares, propelling them by more than 13% to record highs. Over the past two years, the company’s shares have skyrocketed by almost 150%.
These encouraging outcomes could potentially influence insurers in the U.S. and health authorities in Europe to extend coverage of Wegovy to a broader segment of patients. Currently, some healthcare plans, including the U.S. Medicare health plan, categorise weight-loss treatments as lifestyle drugs. Experts opine that the new data might lead to a reassessment of this stance, particularly in the U.S., where the cost of Wegovy stands at $1,300 per month.
The findings from the trial have also prompted discussions regarding the long-term health benefits of the drug, particularly in terms of potentially lowering the overall healthcare burden and the expenses associated with treating heart disease in populations with overweight or obesity. Some experts, like Dr. Jeff Levin-Scherz, a consultant at Willis Towers Watson, remain cautious, suggesting that medical cost savings might be years away. He postulates that the drugs may prove to be cost-effective in improving patients’ lives but may not necessarily reduce their overall healthcare costs.
Large American corporations, which previously covered weight-loss treatments for their employees, have reduced their support due to escalating costs. However, the landmark data from the SELECT trial illustrates Wegovy’s potential to redefine how obesity is perceived and treated, according to Martin Holst Lange, Novo Nordisk’s executive vice president for development.
Novo Nordisk has expressed plans to submit applications for regulatory approvals of a label indication expansion for Wegovy in the U.S. and the European Union within the year.
Wegovy has already had a transformative impact on the weight-loss market since its U.S. introduction in June 2021. It has not only garnered attention from patients, investors, and celebrities around the globe but also significantly contributed to Novo’s shares’ growth. The injection helps patients feel fuller for more extended periods, resulting in an average weight loss of around 15% when coupled with dietary and exercise changes. The drug is part of the GLP-1 agonists class, initially developed to treat type 2 diabetes.
With obesity affecting over 650 million adults globally, a figure that has tripled since 1975, and approximately another 1.3 billion classified as having overweight, the World Health Organization links these conditions to heightened risks of heart disease and diabetes.
Industry analysts, like Sydbank’s Soren Lontoft Hansen, are optimistic that these better-than-expected results will cause a stir among physicians who prescribe anti-obesity drugs. Furthermore, Barclays analysts project that a positive outcome from the study could boost Wegovy’s uptake by 25% by 2030, provided it receives approval for expanded use.
Novo Nordisk is currently facing challenges to meet the soaring U.S. demand for Wegovy. In May, the company announced it was cutting the supply of starter doses to the U.S. market by half to secure supplies for existing patients. Although larger doses were reported to be in short supply by Reuters, Novo has denied such claims.
The detailed data from the trial is scheduled to be presented at a scientific conference later in 2023, and additional details may be revealed when Novo releases its second-quarter results on Thursday.
Read More
Exercise and weight loss combination amplifies battle against obesity and prediabetes
Groundbreaking research conducted at Washington University School of Medicine in St. Louis reveals the tremendous impact of combining regular exercise with a 10% body weight loss in combating obesity and prediabetes. The study found that this combination more than doubles insulin sensitivity compared to weight loss alone, reducing the risk of developing Type 2 diabetes and coronary heart disease.
The researchers initially knew that modest weight loss improves insulin sensitivity, and exercise alone has limited efficacy in aiding individuals with obesity and prediabetes in shedding pounds. However, they were astonished to discover the profound effect that combining a consistent exercise regimen with a 10% reduction in body weight can have on insulin sensitivity.
Published in the journal Nature Metabolism, the findings shed light on the crucial role of exercise in improving overall health outcomes for individuals struggling with obesity and prediabetes.
Dr. Samuel Klein, the senior investigator and director of the Center for Human Nutrition, explained the significance of the study’s results: “Insulin resistance is a major factor that causes Type 2 diabetes, nonalcoholic fatty liver disease, and abnormal blood lipids in people with obesity. We’ve shown that combining exercise with weight loss causes a marked improvement in whole-body insulin sensitivity, thereby lowering the risk of developing diabetes and treating obesity-related metabolic diseases to a much greater degree than is possible with weight loss alone.”
The study involved 16 participants with a body mass index (BMI) ranging from 30 to 49, indicating obesity. All participants had prediabetes and demonstrated medical evidence of insulin resistance.
Eight participants underwent a diet-only intervention, resulting in a 10% body weight loss. The other eight individuals followed the same dietary plan but also engaged in supervised exercise sessions multiple times per week.
Dr. Klein highlighted the significance of their findings: “The data from most studies show that exercise has very little effect on body weight in people with obesity… Our study involved detailed analyses of metabolic changes in muscle and body fat before and after a 10% weight loss in people who lost weight with diet therapy alone and in those who lost the same amount of weight with diet therapy plus supervised exercise training. The results demonstrate that the benefits of combining exercise with weight loss are considerable.”
With over 37 million Americans living with diabetes and more than 40% of the population grappling with obesity, which is a significant contributor to diabetes cases, the study’s findings have far-reaching implications. Approximately 96 million adults in the United States, or one in three, are estimated to have prediabetes.
Dr. Klein emphasised the crucial role of exercise in weight management therapy, stating, “The metabolic benefits we found in this study demonstrate the profound reasons why exercise should always be included in weight-management therapy.”
Read More
Family-focused approach in paediatric primary care proves effective for child weight loss
A groundbreaking family-based treatment for childhood obesity, developed by researchers at the University at Buffalo (UB), has demonstrated significant success in a multicenter study conducted in paediatric primary care settings. Previously available only in specialised clinics, this evidence-based treatment has now been implemented for the first time in four U.S. cities, targeting children aged 6-12 and their parents.
Published in the Journal of the American Medical Association, the study reveals that family-based treatment conducted in paediatricians’ offices leads to improved weight-loss outcomes not only for the treated child and parent but also for untreated siblings. The research, supported by the National Heart, Lung and Blood Institute, emphasises that the healthy behaviours promoted during the treatment extend beyond the immediate family members, potentially improving the overall health of the entire family.
In the study, three times as many children in the treatment group (27%) experienced a clinically meaningful reduction in median body mass index (BMI) compared to the usual care group (9%). These improvements in weight correlated with enhanced cardiometabolic outcomes, such as blood pressure, lipids, and glucose regulation. The success of this novel family-focused treatment, pioneered by senior author Leonard H. Epstein, has significant implications for the long-term health and well-being of the treated children.
The family-based treatment program involves the implementation of eating and activity plans, education in parenting and behavioural techniques, and the facilitation of support for positive behaviour changes within both the family and peer environments. In individualised sessions, parents and children are seen together, reviewing self-monitored eating and activity levels, treatment manuals, handouts, and setting goals for weight and behaviour.
The randomised clinical trial enrolled 452 children aged 6 to 12, with one parent, in primary care practices across Buffalo, Rochester, Columbus, and St. Louis. Half of the children received family-based treatment, while the other half received usual care. Notably, the treatment demonstrated positive outcomes across racial and ethnic backgrounds.
Children receiving family-based treatment showed a significant difference in percent over median BMI compared to those receiving usual care, with a reduction of 6.48%. Furthermore, parents experienced a reduction of 3.97% in BMI, and untreated siblings who were overweight had a reduction of 5.38%. These changes in BMI among family members were interrelated, suggesting that the treatment fosters the modelling of healthy behaviours and facilitates real change in the shared family environment.
The success of this behavioural intervention underscores the growing need for similar treatments in paediatric primary care. The study authors emphasise the necessity for “coaches” in primary care settings who can provide support for obesity treatment and address various behavioural issues, including anxiety, depression, and eating disorders.
The implementation of this family-focused approach not only ensures the immediate health of children but also equips them with lifelong healthy practices. The study’s positive outcomes highlight the potential for transforming paediatric primary care into a hub for comprehensive behavioural interventions, addressing a wide range of health-related concerns.
Read More
Obesity alters brain function, hindering weight loss maintenance, study finds
Researchers from Amsterdam UMC and Yale University have recently unveiled a ground-breaking link between obesity and altered brain responses to nutrients. Their study indicates that obesity leads to reduced dopamine release and diminished nutrient-sensing activity in the brain. Worryingly, these changes persist even after weight loss, potentially explaining why maintaining weight loss is so challenging for many.
The research, published in Nature Metabolism, highlights that the brain’s responses to certain nutrients are impaired in individuals with obesity and don’t show improvement even after shedding weight.
Mireille Serlie, the lead researcher and Professor of Endocrinology at Amsterdam UMC, elaborates on the implications of the study, “Our results point toward enduring alterations in the brain among individuals with obesity, which could have a substantial impact on eating behaviour. We observed that, compared to individuals of normal weight, those with obesity exhibited lower dopamine release in a brain region that plays a pivotal role in the motivation associated with food consumption. Dopamine is crucial for the rewarding aspects of eating. Moreover, those with obesity demonstrated diminished brain activity in response to the infusion of nutrients into the stomach. Collectively, these results suggest that the brain’s ability to sense nutrients in the stomach and gut, or to process nutritional signals, is compromised in obesity, which may have significant repercussions on food intake.”
The regulation of food consumption is dependent on a complex interplay of metabolic and neural signals among the brain and various organs, such as the gut, as well as nutritional signals in the blood. This intricate network governs hunger and satiety sensations, regulates food intake, and controls the motivation to seek food. Though advances have been made in understanding these processes in animals, especially regarding metabolic diseases like obesity, less is known about the human mechanisms, mainly due to challenges in creating experimental setups within clinical settings that can elucidate these processes.
Addressing this knowledge gap, Serlie and her team, including colleagues from Yale, conducted a meticulously designed controlled trial. The study involved 30 participants with obesity and 30 of normal weight. It entailed infusing specific nutrients directly into the participants’ stomachs while simultaneously assessing their brain activity using MRI scans and monitoring dopamine release with SPECT scans.
The study discovered that while participants of normal weight showed distinct patterns of brain activity and dopamine release in response to nutrient infusion, these responses were significantly weakened in those with obesity. Furthermore, even after achieving a 10% body weight loss through a 12-week diet, the brain responses in individuals with obesity did not improve. This finding suggests that obesity induces long-term adaptations in the brain that persist even after weight loss.
“The enduring nature of these brain alterations, which do not reverse even after weight loss, might elucidate why so many individuals tend to regain weight following initial successful weight loss,” Serlie concludes.
This discovery brings to light the intricate challenges faced by those striving to lose weight and maintain the loss, suggesting that strategies need to address not only the physical aspects but also the neurological factors entangled with obesity.
Read More
Weight loss injections could be prescribed to children with obesity
UK government officials are contemplating offering weight-loss injections to children with obesity as young as 12 in an effort to combat the escalating childhood obesity problem in the country.
Specialists are currently evaluating if semaglutide injections, a weight-loss medication recently sanctioned for adult use by the NHS, could be beneficial for children with obesity aged between 12 and 17. Health authorities are now encouraging the National Institute for Health and Care Excellence (NICE) to consider providing these injections to teenagers struggling with obesity.
The final decision, expected to be announced in early 2024, is being supported by experts who argue that the medication could prevent more children from needing invasive weight-loss procedures. However, this suggestion has sparked controversy, with some arguing it could lead to an over-medicalisation of children.
Those opposed to the idea of weight loss injections for children raise several concerns. They fear the potential interference of these drugs with the physical and mental growth and development of children. They also highlight the lack of evidence regarding the long-term effects of such treatments on children’s health.
Critics further argue that such injections might encourage an unhealthy emphasis on weight and physical appearance, potentially leading to body image issues and disordered eating. The potential for serious side effects from weight loss injections is another concern. Additionally, they worry about the psychological message these injections could send, implying that a child’s body is unacceptable as it is.
Professor Keith Godfrey, from the National Institute for Health and Care Research’s Southampton Biomedical Research Centre, warns that providing weight-loss injections to children might lead to the unnecessary medicalisation of an entire generation.
Charlotte Summers from Gro Health, a company offering health and wellbeing programs for adults, children, and young people, advocates for a more holistic approach: “By promoting healthy eating habits, regular physical activity, and a positive relationship with food, we can enable our children to attain and maintain a healthy weight throughout their lives. This comprehensive strategy not only contributes to physical wellbeing, but also lays a solid foundation for emotional and mental health. We must collaborate to support our children in adopting a balanced and wholesome lifestyle for a healthier, brighter future.”
Read More
A good night’s sleep may make it easier to stick to exercise and diet goals, study finds
Preliminary research presented at the American Heart Association’s Epidemiology, Prevention, Lifestyle & Cardiometabolic Health Scientific Sessions 2023 suggests that people who get regular and uninterrupted sleep are more successful at sticking to their exercise and diet plans while trying to lose weight.
The researchers found that good sleep health was associated with higher rates of attendance at group interval sessions, adherence to caloric intake goals and improvement in time spent performing moderate-vigorous physical activity. The researchers examined 125 adults with overweight or obesity over 12 months in a weight loss program that included measurements of sleep habits through patient questionnaires, sleep diaries and wrist-worn devices.
They measured adherence to the program by percentage of group intervention sessions attended, percentage of days that participants ate between 85-115% of their recommended daily calories, and change in daily duration of moderate or vigorous physical activity.
The study’s limitations include that it did not incorporate any intervention to help participants improve their sleep, that the study sample was not recruited based upon participants’ sleep health characteristics, and that the overall sample population had relatively good sleep health at baseline. Additionally, the sample was primarily white and female, so it is unclear whether these results are generalisable to different population groups.
Overall, the preliminary research suggests that sleep may play a key role in promoting self-control and making healthy choices, highlighting the need for public health efforts to promote healthy sleep habits and the importance of getting enough sleep for maintaining a healthy lifestyle.
Read More